We’re on the Case
misconduct allegations, and
government regulation.
State and Federal authorities routinely conduct investigations into the conduct of licensed professionals, such as physicians, attorneys, social workers, nurses, and others who provide sophisticated services to the public. These are government agencies – such as the Office of Professional Medical Conduct, the Attorney Grievance Committees, the Education Department’s Board of Regents, or the Office of Professional Development – who issue licenses to qualified applicants and/or monitor the conduct of those in practice. Complaints from customers, clients, or peers may find their way to these agencies’ investigators.
Even a single report can kickstart a full-blown inquiry into your compliance with rules of conduct and ethics in your profession. A simple request for patient records can lead to a wide-ranging investigation into your professional practices. Have you documented your habits and due diligence? Are there clients, patients, or colleagues who would speak poorly of your performance? A review from a body like the Office of Professional Medical Conduct (OPMC) or the Education Department’s Office of Professional Discipline (OPD) could result in suspension, fines, or license revocation.

Prescribing Opioids? Click here for a summary of the most recent CDC GuidelineThe Linehan Law Firm assists professionals in answering before these licensing and professional boards in the wake of a variety of accusations. Most professionals stand proudly by their practices, and eagerly wish to defend themselves against unfounded allegations. But early legal representation is paramount to create a shield between your practice and government authorities. Demands for medical files, client communications, patient information or billing records can all be part of a greater investigation unknown to even the most diligent of professionals. Any response provided in answer to these demands can be used against you in future proceedings. Discipline defense counsel can seek clarity on the issues involved, negotiate a fair settlement or compromise with the authorities, employers, or any third parties involved, and connect clients to professional assistance, if necessary. Complaints from clients or patients – particularly in the age of online social media – can easily turn into a public relations nightmare for a busy professional.
Notice from the OPMC will be sent my mail to your office, and will look something like this:
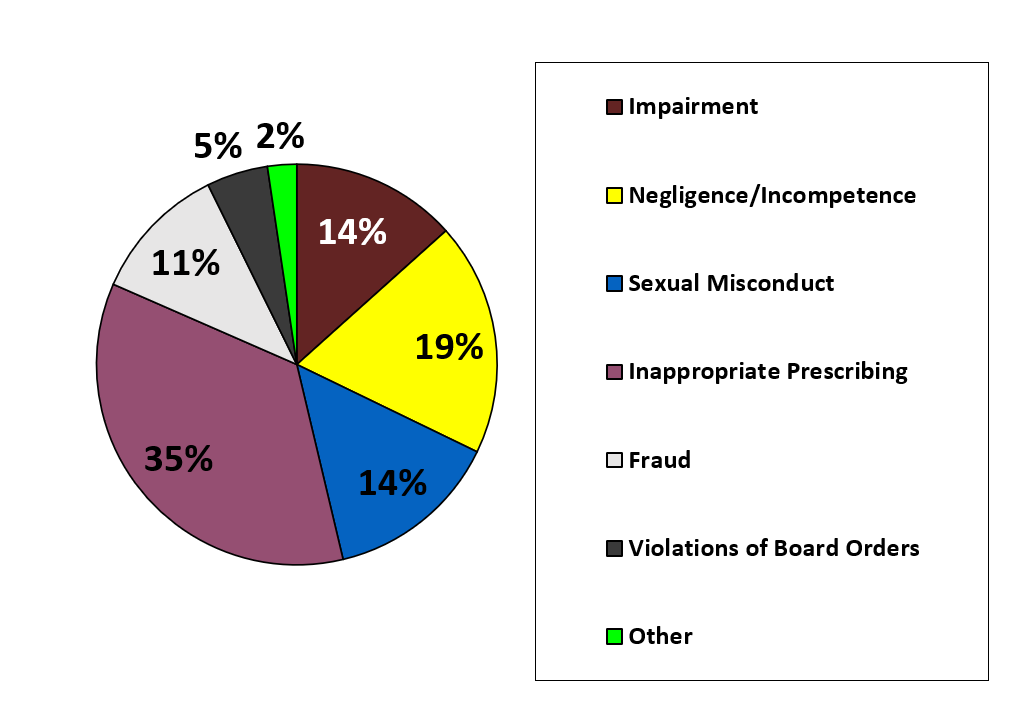
For physicians, nurse practitioners, and physician assistants, OPMC investigates claims of negligence, incompetence, criminal allegations, and other misconduct. These investigations may include interviews of patients, staff, and colleagues, audits of medical files and billings to insurance carriers, and possibly an administrative hearing visible to the public. In 2020 alone, OPMC received over 7,900 complaints, and moved forward to disciplinary proceedings with over half of them. Almost half come from members of the public. Improving patient relations and keeping up with government requirements will save you considerable time and expense.
Complaints are often initiated from reviews of medical malpractice websites, media reports, or OPMC’s review of prescription records. OPMC staff review and evaluate available evidence and may contact physicians for an interview or to obtain documents. You have the right for an attorney to be involved in this process, but OPMC also has authority to request medical records in your possession. Medical experts board certified in specific areas of practice usually review records as part of the OPMC investigatory process and identify whether the physician under review met minimum standards of care. If enough evidence of misconduct is brought before the Board and the OPMC director, and if the case is not resolved by a physician’s attorney advocating on their behalf, a committee will vote to refer cases for formal charges. The physician under scrutiny will be advised and the charges will be made public within 5 days.
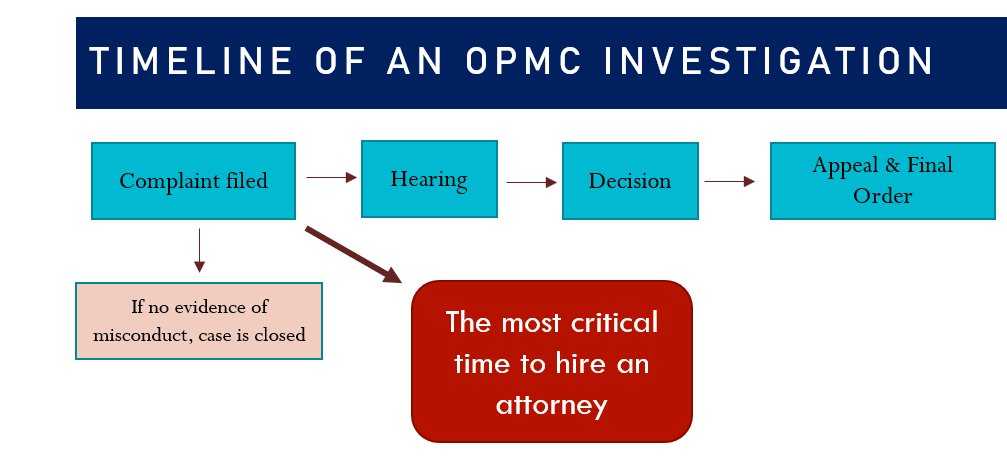
If an investigation proceeds to a hearing, the Commissioner of Health will order a physician’s license to be suspended pending the outcome of the hearing. Even if a physician appeals a Board order, the suspension will not be postponed.
If the investigation’s findings are adopted by the State Board for Professional Conduct, it can penalize practitioners with fines of up to $10,000, probationary periods, limitations on your practice areas, community service, and suspension or revocation of your license.
Many practitioners avoid a formal disciplinary hearing by entering into “consent agreements” with the Board, which usually include compromises on penalties and conditions on the physician’s practice. These resolutions may not always be ideal, but they save one’s time, legal fees, and may be the best way to keep one’s license.
The vast majority of OPMC actions end with serious consequences for physicians.
If a practitioner’s license is suspended, it can later be restored upon a showing that the licensee has been rehabilitated, completed a prescribed course of treatment, or fulfilled other requirements.
For nurses, pharmacists, social workers, and dentists, the New York State Department of Education’s Office of Professional Discipline conducts similar but less formal investigations often based on phone calls or interviews made to the professionals under investigation, who are required to submit records for review within 30 days of notice. OPD makes recommendations to the Board of Regents, which can impose penalties like public reprimands, up to $10,000 fines, suspension and revocation of your license.
Disciplinary actions can have long-lasting repercussions on your reputation. Let’s talk about keeping your practice secure.